Diverticulitis is an inflammatory gastrointestinal condition of the large intestine (colon) that causes problems like bloating, constipation, abdominal pain, fever, diarrhea, and nausea.
It is a common disease that occurs when people age. Diverticulitis is more prevalent in the US, but it is increasing worldwide.
Doctors prescribe antibiotics, acetaminophen, and tricyclic antidepressants to treat this, but certain drugs may increase or worsen symptoms, which can lead to surgery.
So, in this article, we will discuss what drugs to avoid diverticulitis, along with more necessary information.
What Is Diverticulitis?
Diverticulitis is a condition where the lining of the colon becomes infected and inflamed at the area of small outpouchings called diverticula.
In other words, small pockets or bulges (diverticula) develop in the colon's lining (large intestine), causing symptoms like abdominal pain, constipation, bloating, diarrhea, fever, and nausea.
The main reason behind this condition is increased pressure in the colon areas where the wall is weak. Diverticula disease is more prevalent in people over 40.
When the diverticula becomes infected or inflamed, it becomes harmful. According to some experts, the bacteria present in the gut enter the diverticula and cause infection.
This infection is called diverticulitis, causing abdominal pain, increased white blood cells, and generalized malaise.
This condition can be treated with antibiotics and bowel rest. But sometimes, when the complications reach a bowel abscess, perforation, fistula, or obstruction, it is treated with surgery.
What Are Diverticulitis Symptoms?
Some common signs of diverticulitis are:
- Abdominal pain.
- Tiredness.
- Stomach aches.
- Swelling or bloating.
- Fever or nausea.
- Changes in bowel movements.
Remember, these are the common symptoms that can also occur from other gastrointestinal conditions like irritable bowel, inflammatory bowel disease, and more. To properly diagnose, get help from your doctor.
Diverticulitis Risk Factors
Low fiber intake may trigger the attack of diverticulitis. Taking a proper amount of fiber is essential for a healthy digestive system because it adds bulk to your stool and helps to move it to the digestive tract. So, include foods that are rich in fiber.
Your risk of diverticulitis can also trigger when:
- Age: Diverticular disease is more common as people age, especially after 40.
- More red meat consumption: Consuming more red meat can result in an increased risk of diverticular disease.
- Less exercise: Doing less exercise can increase the risk of diverticulation. Try weight-bearing exercise to prevent this disease.
- Low-fiber diet: Eating more low-fiber foods may increase the risk of diverticular disease.
- Having obesity: A diagnosis of obesity is connected to a higher rate of diverticulitis.
- Smoking cigarettes: Smoking can lead to diverticular disease and diverticulitis symptoms.
Drugs to Avoid With Diverticulitis
Many factors can cause diverticular disease, like diet, lifestyle, genes, or bacteria present in the gut. But in some cases, some drugs/medicines can also raise the trigger risk of diverticulitis, causing bleeding and perforations (holes) in the intestine.
Below, we have mentioned some medications that need to be avoided in diverticulitis:
i). Steroids
According to the studies, steroids like corticosteroids and prednisone increase the risk of diverticulitis. Prolonged taking of corticosteroids increases the risk of bowel perforations.
ii). Opioids
According to the studies, taking opioids like codeine, hydromorphone, morphine, Opana (oxymorphone), OxyContin (oxycodone), and Vicodin (hydrocodone) increases the risk of complications of diverticulitis like bleeding, abscess formation, sepsis, fistula formation, and obstruction.
iii). Calcium channel blockers
According to this study, taking some common calcium channel blocker drugs like Cardene (nicardipine), Cardizem (diltiazem), Procardia (nifedipine), Norvasc (amlodipine), and Verelan (verapamil) can lower the blood pressure.
These drugs also increase the risk of bleeding and perforations, causing diverticulitis.
iv). Nonsteroidal anti-inflammatory drugs (NSAIDs)
People who take OTC NSAIDs like Advil or Motrin (ibuprofen) and Aleve or Naprosyn (naproxen) have a higher risk of bleeding with diverticula.
v). Antihistamines
According to this study, taking antihistamines can treat diverticulitis complications, but one study indicated that they can increase the risk of intraabdominal abscess formation.
vi). Tricyclic antidepressants
According to the Mayo Clinic, consuming tricyclic antidepressants can cause constipation, leading to diverticulitis.
vii). Iron supplements
According to this study, iron supplements like ferrous sulfate can cause a high risk of gastrointestinal effects, including constipation. Even case reports show that iron supplements can lead to ileus (temporary paralysis of the small intestine) to bowel obstruction from constipation.
How to Prevent Diverticulitis From Recurring?
Diverticulitis can become severe once they are inflamed and may require serious surgery. But it may still reoccur. Thankfully, there are some ways through which you can stop this from rehappening:
- Exercise: Find activities that you enjoy and get moving. Do at least 150 minutes of light exercise, like walking, or 75 minutes of high-intensity aerobic exercise per week, like running, cycling, or swimming.
- Include more fiber: After your body has healed from diverticulitis, consume more fiber-rich fruits and vegetables to help prevent the disease from recurring.
- Take a probiotic: These supplements promote the growth of good gut bacteria, potentially helping protect against diverticulitis.
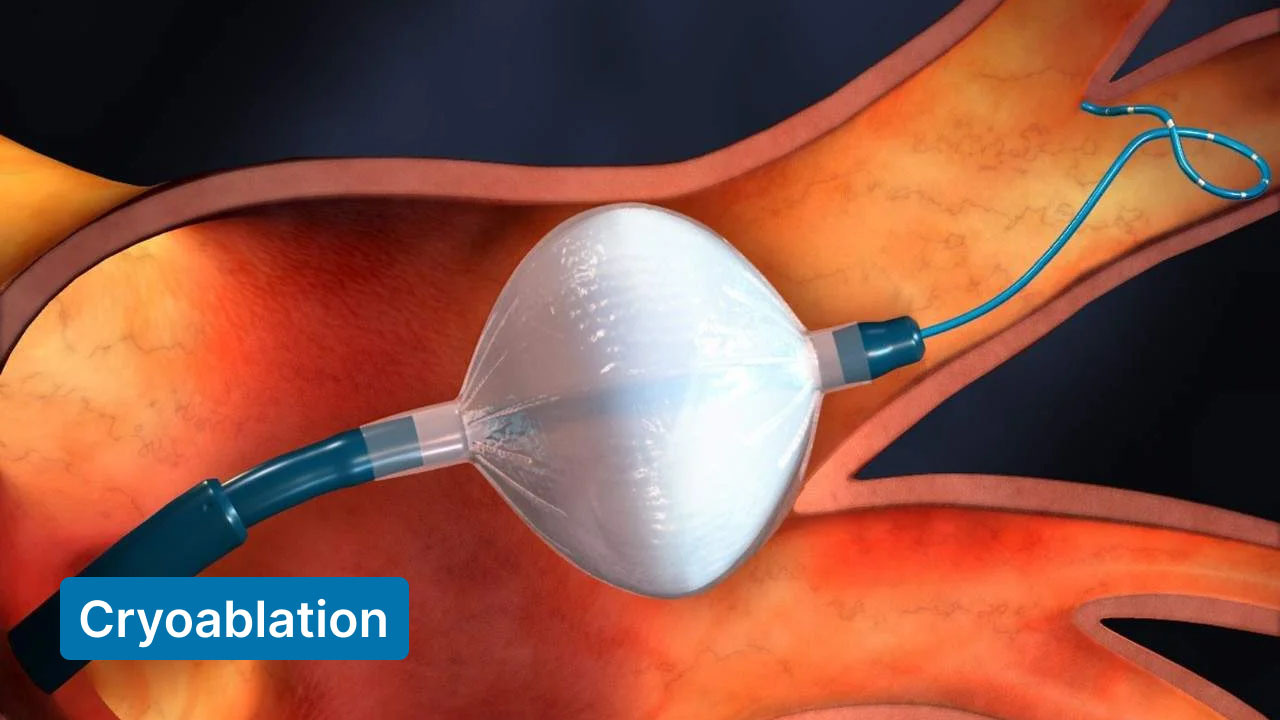
Treatments for Complex Diverticulitis
Uncomplicated diverticulitis can be treated just by visiting the doctor, but complicated diverticulitis needs advanced diverticulitis treatment. Diverticulitis becomes complicated when it includes perforation, abscess, fistula, intestinal obstruction, or bleeding.
If these symptoms are present, they must be treated in the hospital through surgery.
Here are some expected treatments that are used in severe cases of diverticulitis.
-
Intravenous Antibiotic or Pain Therapy
Suppose a person has a weak immune system. In that case, there are chances that they are asked to be hospitalized and treated with antibiotics intravenously and pain medicine by connecting a tube to your vein.
In intravenous therapy, medicine is supplied to the bloodstream and works faster.
-
Surgery
In the case of complex diverticulitis, the doctor may discuss the possibility of surgery. Surgery is recommended in two cases:
- Perforation, abscess, fistula, or intestinal blockage.
- Severe diverticulitis can only be treated with surgery.
Surgery aims to remove diseased colon sections. The first approach is bowel resection. It is the process of removing the affected colon section and reconnecting healthy colon sections to regain normal bowel function. This process can be done with open surgery or a laparoscopic procedure.
The second treatment approach is bowel resection with colostomy, which can only be performed when the first approach is impossible. The process is more severe as a hole or opening for the large intestines is created through the abdominal wall.
Your surgeon connects a temporary bag at the end of this opening, which collects waste. When the diverticulitis heals, the surgeon will reconnect your colon.
What Is The Best Diverticulitis Medication?
There are some drugs/medications available for diverticulitis. However, according to some new studies, mild cases of diverticulitis disease do not need medicines, and they can be cured on their own with time.
However, if you experience diverticulitis symptoms, contact your healthcare provider and share your complete health history and all your discomforts. Your doctor will prescribe you with some medicines.
Mainly, prescribed antibiotics include:
- Augmentin
- Flagyl
- Cipro
However, antibiotics are short-term solutions, and you must focus on your lifestyle to prevent this disease. Follow the complete course once antibiotics are prescribed, even if you feel good.
How To Treat Diverticulitis Without Prescription Medication?
Diverticulitis pain slowly goes away in a few days or weeks. However, some ways do not require any medications for instant relief from the pain.
a). Diet
As the symptoms of diverticulitis start, it is recommended to take a liquid and low-fiber diet, as high-fiber food can cause discomfort or bloating at the start of the disease, and slowly add more nutrition to your diet, from low-fiber to high-fiber food. So, gradually scale up your diet.
b). Heating Pad
Another way is to use a heating pad. This method is simple and quickly reduces abdominal discomfort. Follow the instructions on the heating pad to cope with the pain. Do not fall asleep while using a heating pad.
c). Try Probiotics
Due to the presence of gut bacteria species in probiotics, they help with digestive conditions. According to a 2016 review, probiotics may reduce symptoms and recurrence of diverticular disease.
Including probiotic supplements like yogurt, kefir, sauerkraut, miso, and kimchi can be helpful. However, probiotics can sometimes cause side effects, like gas, bloating, and diarrhea, so take them in moderation.
d). Do More Exercise
Exercise helps reduce the pain of diverticulitis by releasing endorphins. The Physical Activity Guidelines for Americans suggest that adults do at least 2 hours and 30 minutes of moderate-intensity weekly exercise.
Summary
Remember that diverticular disease is partly genetic and can not be entirely avoided. Prescription drugs affect the development of diverticulitis.
Some recommend antibiotics to treat diverticulitis, but it is only sometimes helpful. Pain-reducing medicines can also help, but take them after the consultation with your healthcare.
To reduce its effects naturally, try to change your lifestyle, consume a healthy diet, take proper medical care, and exercise regularly.
FAQs
1. What can worsen diverticulitis?
Ans: Lack of low fiber intake can cause symptoms of diverticulitis, leading to constipation and strain of the bowel. Also, lifestyle plays a major role in flare-ups of diverticulitis.
2. What medications irritate diverticulitis?
Ans: People with diverticular complications should be careful about specific drugs' possible risks and benefits. Medicine like aspirin or NSAIDs can increase the risk of diverticulitis and diverticular bleeding.
3. How do you calm diverticulitis naturally?
Ans: To naturally treat diverticulitis, include a liquid diet and increase your consumption of fiber and anti-inflammatory foods. Try to avoid red meat and high-fat foods, alcohol, and take some fiber supplements.
4. How do you stop diverticulitis from advancing?
Ans: A high-fiber diet like fresh fruits, vegetables, and whole grains helps stool pass quickly through your colon and can help prevent diverticulitis. But if it is just the starting stage, avoid a high-fiber diet. Consulting a doctor and getting some antibiotic medication are first-line treatments.
Read Also: